UArizona Researchers Near Trials of First Drug for Vascular Dementia
University of Arizona Health Sciences researchers are moving closer to conducting clinical trials on what would be the first therapeutic drug for vascular cognitive impairment and dementia (VCID), the second most common form of dementia after Alzheimer’s disease.
To date, the U.S. Food and Drug Administration has not approved any drugs that specifically treat vascular dementia, which involves cognitive impairment caused by injuries – often stroke related – to the vessels supplying blood to the brain.
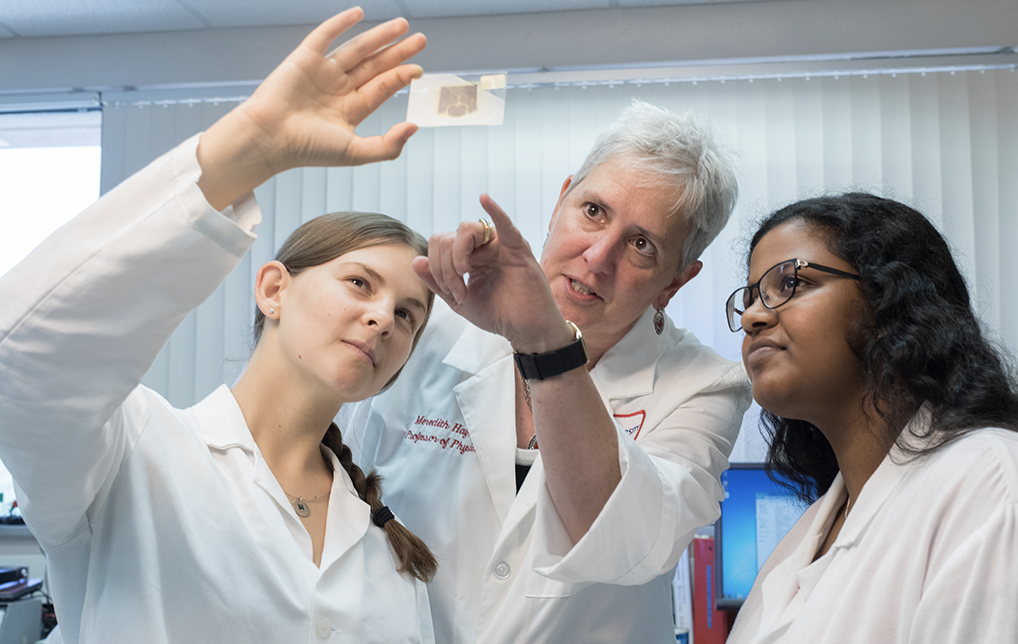
Meredith Hay, PhD, professor of physiology at UArizona College of Medicine – Tucson and a faculty member in the Evelyn F. McKnight Brain Institute , is principal investigator of a $5.7 million federal grant from the National Institute for Aging (NIA), part of the National Institutes of Health (NIH). The NIA/NIH grant will allow Dr. Hay and her research team to begin human trials on a novel peptide therapeutic they developed to treat cognitive impairment.
In previous studies, the peptide Dr. Hay and her team created, known as PNA5, decreased brain inflammation and improved brain blood flow to protect brain function, showing great promise as a candidate for treating VCID and other inflammation-related brain diseases. Results were published in the Journal of Pharmacology and Experimental Therapeutics.
“Inflammation-related brain disorders such as vascular dementia affect countless lives and families, yet no FDA-approved therapies exist for these conditions,” said University of Arizona President Robert C. Robbins, MD. “This novel drug candidate being developed by Dr. Hay and her team continues the University of Arizona’s strong history of excellence in understanding the aging brain and is why we have made one of the most pervasive health care problems of our time a strategic priority. The university is committed to improving human health and wellness at every opportunity, and I look forward to seeing what Dr. Hay and her team will do.”
“No family goes untouched by cognitive impairment and diseases leading to increased risk for Alzheimer’s disease,” said Dr. Hay, who also is a member of the Sarver Heart Center and BIO5 Institute at UArizona. “This new therapy has significant potential for treating these diseases and improving the lives of millions of patients and their families.”
After Alzheimer’s disease, vascular dementia is the most common form of dementia and is involved in nearly half of all dementia cases. Vascular dementia occurs when the vascular system is disturbed and blood flow is restricted, starving the brain of oxygen and nutrients. When the brain lacks adequate amounts of blood flow, containing oxygen and nutrients, brain cells begin to die.
Increased brain inflammation and decreased brain blood flow accelerate the progression of vascular dementia. Risk factors for the disorder include hypertension, diabetes and heart failure, and coexisting conditions related to atherosclerosis (coronary artery disease, peripheral artery disease). Other non-Alzheimer’s dementias linked to brain inflammation include dementias associated with pre-Alzheimer’s, multiple sclerosis and Parkinson’s disease.
PNA5 works as a natural anti-inflammatory and neuroprotectant – a therapy intended to prevent damage to the brain or spinal cord from ischemia, stroke, convulsions or trauma – by increasing brain blood flow, decreasing reactive oxygen species (ROS) production, and decreasing pro-inflammatory mechanisms that accelerate the progression of neurodegenerative disease. ROS are chemically reactive chemical species that contain oxygen, such as peroxides, superoxide and hydroxyl radicals, that may lead to oxidative stress that can damage structures inside brain cells. PNA5 also has shown efficacy in treating both pain and cognitive impairment associated with traumatic brain injury.
Collaborating on the research are UArizona faculty members:
- John Konhilas, PhD, associate professor, Department of Physiology, College of Medicine – Tucson;
- Heidi Mansour, PhD, RPh, associate professor, Department of Pharmacology and Toxicology, College of Pharmacy; and
- Robin Polt, PhD, professor, Department of Chemistry and Biochemistry, College of Science and College of Medicine – Tucson.
Dr. Hay, president and founder of ProNeurogen Inc., a Tucson biotechnology company that licenses the technology from UArizona, said the team hopes to conduct human clinical trials with this dementia therapeutic in about three years.
Research reported in this publication was supported by the National Institute on Aging, a unit of the National Institutes of Health, under Award No. 1U01AG066623-01.





